Uterine inversions of tumor origin in two cases at the Joliot Curie Institute at the Aristide Le Dantec University Hospital Center
Inversions utérines d’origine tumorale dans deux cas à l’Institut Joliot Curie du CHU Aristide Le Dantec
S. Ka1, A. Diakhaté1, D. Diop1, RO. Somé2, AC. Diallo1, M. Bah1, ME. Charfi1, A. Dem1.
1 Institut Joliot Curie de Dakar, Sénégal.
2 Souro Sano teaching hospital, Burkina Faso.
DOI: 10.54266/ajo.2.1.42.SpbwgLIjTv
ABSTRACT
INTRODUCTION: Non-puerperal uterine inversions are a rare situation. Indeed, 85% of uterine inversions are puerperal. We report two cases observed at the Joliot Curie Institute of the Aristide le Dantec University Hospital. OBSERVATIONS: It was about a 39-year-old primigravida and a 47-year-old seventh gestational patient, who had a stage 4 of uterine inversion picture in relation to uterine sarcoma and uterine myoma respectively. The diagnosis was suspected at the clinic due to the absence of palpation of the uterus. Confirmation was made on medical imaging and intraoperatively. Management was radical with a total hysterectomy with bilateral adnexectomy via the vaginal and abdominal routes. However, in the first patient with sarcoma, surgery combined bilateral pelvic lymphadenectomy and was preceded by chemotherapy. CONCLUSION: Non-puerperal uterine inversion is a rare situation. Its treatment is essentially surgical. However, it is important to look for an etiology and in the case of a tumor to ensure that the mass is a cancer or not because the management and prognosis depend on it.
KEYWORDS: Uterine inversion; Uterine sarcoma; Vaginal mass.
RESUME
INTRODUCTION : Les inversions utérines non puerpérales sont une situation rare. En effet, 85% des inversions utérines sont puerpérales. Nous rapportons deux cas observés à l’Institut Joliot Curie du CHU Aristide le Dantec. OBSERVATION : Il s’agissait d’une primigeste de 39 ans et d’une patiente de 47 ans en septième gestation, qui présentaient respectivement un tableau d’inversion utérine de stade 4 en relation avec un sarcome utérin et un myome utérin. Le diagnostic a été suspecté à la clinique en raison de l’absence de palpation d’utérus. La confirmation a été faite sur l’imagerie médicale et en peropératoire. La prise en charge a été radicale avec une hystérectomie totale avec annexectomie bilatérale par voie vaginale et abdominale. Cependant, chez la première patiente atteinte de sarcome, la chirurgie associait une lymphadénectomie pelvienne bilatérale et était précédée d’une chimiothérapie. CONCLUSION : L’inversion utérine non puerpérale est une situation rare. Son traitement est essentiellement chirurgical. Cependant, il est important de rechercher une étiologie et en cas de tumeur de s’assurer que la masse est cancéreuse ou non car la prise en charge et le pronostic en dépendent.
MOTS-CLES : Inversion utérine ; Sarcome utérin ; Masse vaginale.
INTRODUCTION
Non-puerperal uterine inversion is an uncommon disease (1). Indeed, 85% of uterine inversions have puerperal origin (2). Depending on the severity, four degrees can be distinguished (2): first degree (the uterine fundus is depressed in a “vial bottom” or cup), second degree (the uterus is inverted and passes through the external cervical opening), third degree (the uterine body becomes intravaginal and can completely externalize) and fourth degree or total inversion (the vaginal walls participate in the inversion). We report two cases of uterine inversion with tumoral origin observed at the Joliot Curie Institute in Dakar.
OBSERVATIONS
Case 1: It was about a primigravida, primiparous 39 years old woman, without particular pathological background, who had consulted for hydrorrhea. The clinical examination had found a good general status, an abdominal and pelvic mass going up two fingertips above the umbilicus. The vulva was soiled with serum with the presence of a necrotic mass developed at the expense of the uterus. Histological examination of the biopsy specimen was in favor of a sarcomatous tumor. Abdominal and pelvic ultrasonography had found a uterine mass that measured 112x83x78 mm with no impact on the upper urinary tract. The thoracic and abdominal pelvic CT-scan found a uterine tumor prolapsing in the vagina infiltrating the anterior surface of the rectum and pushing the bladder back without any obvious sign of invasion and without any distant metastasis. Pelvic MRI found a cervical tumor extending to the posterior myometrium. The diagnosis of uterine sarcoma invading the lower third of the vagina was retained. After tumor board discussion, chemotherapy was administered without clinical response, followed by surgery including abdominal pelvic lymphadenectomy and bilateral adnexectomy followed by vaginal hysterectomy (Figure 1).
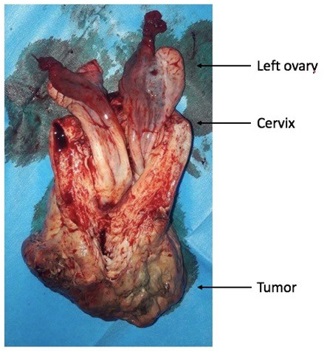
At five months follow-up, there was no particularities.
Case 2:
This was a 47 years old woman seventh gesture with no particular disease background, who had consulted for abdominal and pelvic pain and metrorrhagia. Clinical examination revealed a third-degree uterine inversion with a mass appended to the uterine fundus (Figure 2A). Histology of the biopsy specimen was in favor of a fleshy bud. At the pelvic ultrasound, the uterus was not visualized. We found a rounded anechoic image with sharp storytellers, located behind the five cm long. The diagnosis of a type 4 uterine inversion associated with an ovarian cyst was made. Management included a hysterectomy with bilateral adnexectomy in two stages. A stage of abdominal approach with control of ovaries which are aspirated through the inverted uterine hole and a stage of vaginal approach (Figure 2B).
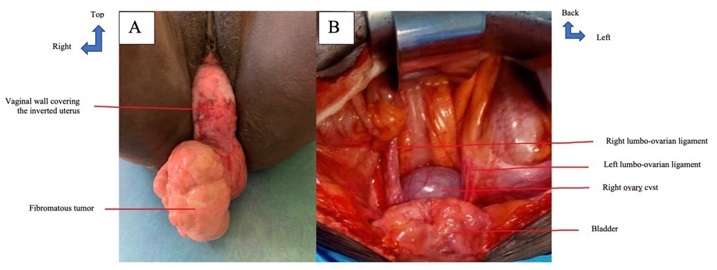
Surgical suites were without any complications. Histological examination of the surgical specimen showed a uterine leiomyoma.
DISCUSSION
Uterine inversion is defined as an invagination of the uterine fundus like a “glove finger”. It is an exceptional clinical situation, especially outside the puerperal period (3). Between 1976 and 2014, only fifty-six cases have been recorded in the literature and mainly concerned menopausal women or women over 45 years of age (4). In our series, we had one patient aged 47 and one aged 39. The diagnosis is made clinically in patients with advanced stages of uterine inversion. It is more precise in intraoperative period (2). Several factors are involved in the physiopathology of non-puerperal uterine inversion: uterine tumor located preferentially on the uterine fundus, thin uterine wall, uterine tumors with small pedicle, rapid tumor growth and wide opening cervix (2). In fact, submucosal myoma is the most found etiology counting for 70 to 85% of cases against 15 to 30% for malignant factors. Between them sarcomas are the most frequent (5). Hysterectomy remains the preferred treatment and/or in case of third or fourth degree uterine inversion (2). It can be performed vaginally (3,6) after careful repositioning of the uterus in its anatomical position (4) which is impossible for fixed and malignant lesions for which carcinologic rules such are resection margins and extensive surgery are essential. A laparoscopy-vaginal route association has also been described by some authors such as Auber et al (7) and Komorek et al (2).
CONCLUSION
Non-puerperal uterine inversion is a rare situation. Its treatment is essentially surgical. However, it is important to look for an etiology and in the case of a tumor to ensure that the mass is a cancer or not because the management and prognosis depend on it.
CONFLICTS OF INTEREST: The authors have declared no conflict of interest.
STATEMENTS
Written informed consent was obtained from the patients for their anonymized information to be published in this article.
Patients confidentiality is protected according to our local institutional ethic committee board considerations.
Patients were informed that data concerning the case would be submitted for publication. They agreed to this. The study followed our hospital investigation guidelines.
Our data are available in the archives of the “Institut Joliot Curie” of teaching hospital of Aristide le Dantec. The data used during the current study are available from the corresponding author on reasonable request.
Funding: None.
S. Ka made the study design and write the paper. All authors were involved in the patient’s management: S. Ka, A. Diakhaté, D. Diop and ME. Charfi for diagnostic, S. Ka, A. Diakhaté, D. Diop, OR. Somé and ME. Charfi, for surgery, AC. Diallo, M. Bah for anatomopathological studies, A. Dem for patients’ evaluation and checking the draft of manuscript. They all reviewed and approved the paper. The authors would like to thank the team of gynecology department of Teaching hospital of Aritide le Dantec for his contribution in management of the patient.
REFERENCES
- DAS. Inversion of the uterus. J Gynaecology Br Emp. 1940;47:525–48.
- Pelissier-Komorek A, Lucereau-Barbier M, Diab J, Gavillon N, Graesslin O. Inversion utérine non puerpérale aiguë du 3e degré. Gynécologie Obstétrique & Fertilité. 2013 Feb;41(2):130–2. DOI : 10.1016/j.gyobfe.2012.12.006
- Atalay MA, Cetinkaya Demir B, Solak N, Oz Atalay F, Kucukkomurcu S. An unusual presentation of a submucous leiomyoma accounting to a non-puerperal uterine inversion: A case report. J Turkish German Gynecol Assoc. 2013 Jun 10;14(2):116–8. DOI : 10.5152/jtgga.2013.55631
- Lupovitch A, England ER, Chen R. Non-puerperal uterine inversion in association with uterine sarcoma: Case report in a 26-year-old and review of the literature. Gynecologic Oncology. 2005 Jun;97(3):938–41. DOI : 10.1016/j.ygyno.2005.02.024
- Kopal Ş, Seçkin NC, Turhan NÖ. Acute uterine inversion due to a growing submucous myoma in an elderly woman: case report. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2001 Nov;99(1):118–20. DOI : 10.1016/s0301-2115(01)00346-3
- Tuckett JD, Yeung A, Timmons G, Hughes T. Non-puerperal uterine inversion secondary to uterine sarcoma and ascites demonstrated on CT and MRI. European Journal of Radiology Extra. 2010 Sep;75(3):e119–23. DOI : 10.1016/j.ejrex.2010.06.008
- Auber M, Darwish B, Lefebure A, Ness J, Roman H. Management of nonpuerperal uterine inversion using a combined laparoscopic and vaginal approach. American Journal of Obstetrics and Gynecology. 2011 Jun;204(6):e7–9. DOI : 10.1016/j.ajog.2011.01.024